Neurofeedback therapy targets the symptoms of Borderline Personality Disorder by focusing on regulating brain activity. By using real-time monitoring of brainwave patterns, neurofeedback aims to train the brain to self-regulate and stabilize emotional responses. This can be particularly beneficial for individuals with BPD who often experience intense mood swings, impulsivity, and difficulty regulating emotions. Through neurofeedback, individuals can learn to modulate their brain activity, leading to improved emotional control and reduced symptom severity.
The potential long-term benefits of using neurofeedback as a treatment for Borderline Personality Disorder include sustained improvements in emotional regulation, reduced impulsivity, and enhanced overall well-being. Respiration Rate As individuals continue with neurofeedback sessions, they may experience lasting changes in their brain function, leading to more stable emotional responses and improved coping mechanisms. This can contribute to better interpersonal relationships, increased resilience to stress, and a higher quality of life for individuals with BPD.
Neurofeedback for Substance Use Disorders (e.g., Addiction Treatment)
Specific neurofeedback protocols and techniques have shown particular effectiveness for individuals with Borderline Personality Disorder. For example, protocols targeting the regulation of specific brainwave frequencies, such as alpha and theta waves, have been found to be beneficial in addressing emotional dysregulation and impulsivity. QEEG (Quantitative EEG) Additionally, neurofeedback techniques that focus on enhancing executive function and cognitive control can help individuals with BPD manage their emotions more effectively.
Neurofeedback therapy addresses the emotional dysregulation commonly associated with Borderline Personality Disorder by directly targeting the underlying brain activity patterns that contribute to these symptoms. Skin Temperature By providing real-time feedback and rewards for desired brainwave patterns, neurofeedback helps individuals learn to self-regulate their emotional responses. This can lead to a reduction in the intensity and frequency of emotional outbursts, as well as an overall improvement in emotional stability.
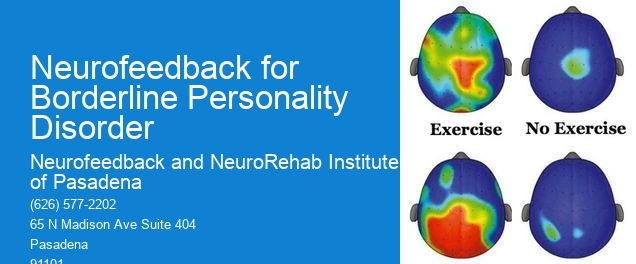
Research and studies have been conducted to support the use of neurofeedback for Borderline Personality Disorder. These studies have demonstrated the effectiveness of neurofeedback in reducing symptoms of emotional dysregulation, impulsivity, and mood instability in individuals with BPD. Additionally, neuroimaging studies have shown changes in brain activity following neurofeedback training, providing further evidence of its impact on brain function.
Neurofeedback can be used as a standalone treatment for Borderline Personality Disorder, although it is often used in conjunction with other therapies for comprehensive care. Baseline When combined with other therapeutic approaches such as dialectical behavior therapy (DBT) or cognitive-behavioral therapy (CBT), neurofeedback can complement the overall treatment plan and enhance the effectiveness of addressing BPD symptoms from multiple angles.
There are minimal potential risks associated with using neurofeedback for individuals with Borderline Personality Disorder. However, it is essential for practitioners to conduct a thorough assessment and ensure that individuals do not have any underlying conditions that may contraindicate neurofeedback. Additionally, working with qualified and experienced neurofeedback providers can help mitigate any potential risks and ensure the safe and effective use of this therapy for individuals with BPD.
Theta Waves
Neurofeedback protocols for social anxiety in teenagers may differ from those for adults due to the unique developmental and cognitive factors at play. When designing protocols for teenagers, practitioners may consider incorporating age-appropriate feedback mechanisms and targeting specific neural networks associated with adolescent social cognition and emotional regulation. Additionally, the protocols may emphasize building skills for managing peer interactions and navigating social challenges commonly faced during adolescence. In contrast, protocols for adults may focus on addressing long-standing patterns of social anxiety and may involve targeting different neural pathways and cognitive processes. Tailoring neurofeedback protocols to the specific developmental stage and cognitive needs of the individual can optimize the effectiveness of the intervention for social anxiety in both teenagers and adults.
Neurofeedback protocols for stroke rehabilitation typically involve a combination of sensorimotor rhythm (SMR) training, beta training, and alpha-theta training. SMR training focuses on enhancing sensorimotor integration and motor function, while beta training aims to improve attention, executive function, and cognitive processing. Alpha-theta training is often used to address emotional regulation and stress management. Additionally, protocols may include coherence training to enhance communication between different brain regions and improve overall brain function. These protocols are tailored to the individual's specific needs and may be adjusted based on the stage of stroke recovery and the areas of impairment. It's important to note that neurofeedback should be integrated into a comprehensive rehabilitation program and supervised by qualified healthcare professionals to ensure safety and effectiveness.
Neurofeedback therapy has shown promising long-term effects in the treatment of ADHD in children. Research indicates that sustained improvements in attention, impulse control, and executive functioning can be observed following a course of neurofeedback sessions. Additionally, studies have suggested that these benefits may endure beyond the immediate treatment period, contributing to enhanced academic performance, social interactions, and overall quality of life for children with ADHD. Furthermore, neurofeedback therapy has been associated with reduced reliance on medication and a lower risk of adverse side effects, offering a non-invasive and sustainable approach to managing ADHD symptoms in the long term.
Neurofeedback has shown promise in providing sustained relief from chronic migraine headaches by targeting the dysregulated brainwave patterns associated with migraine pathophysiology. Through the use of electroencephalogram (EEG) monitoring and real-time feedback, neurofeedback aims to modulate cortical excitability, enhance self-regulation, and promote neuroplasticity. By addressing aberrant neural activity, promoting relaxation, and improving cognitive function, neurofeedback may offer long-term alleviation of migraine symptoms. Additionally, the technique has been found to potentially reduce medication reliance and enhance overall quality of life for individuals suffering from chronic migraines. Furthermore, research suggests that neurofeedback may have a positive impact on comorbid conditions such as anxiety and depression, which are often associated with chronic migraine. Overall, neurofeedback presents a promising avenue for sustained relief from chronic migraine headaches, offering a non-invasive and potentially effective therapeutic approach.
Neurofeedback strategies for substance use disorders can be tailored to address specific neurobiological and psychological factors associated with different types of substance abuse. For instance, for individuals with alcohol use disorder, neurofeedback may focus on enhancing executive function, emotional regulation, and stress management to address underlying cognitive and emotional dysregulation. In contrast, for individuals with stimulant use disorder, neurofeedback interventions may target impulsivity, attentional control, and reward processing to address the unique neurocognitive deficits associated with stimulant abuse. Additionally, neurofeedback protocols may also consider comorbid conditions such as anxiety, depression, or trauma, and incorporate strategies to address these co-occurring factors. By customizing neurofeedback approaches to the specific neurobehavioral profiles and clinical presentations of individuals with substance use disorders, clinicians can optimize the effectiveness of neurofeedback interventions in promoting sustained recovery and relapse prevention.
Yes, there are variations in neurofeedback approaches for different substance use disorders. Neurofeedback techniques can be tailored to address the specific neurobiological and cognitive patterns associated with different substances, such as alcohol, opioids, stimulants, or cannabis. For example, neurofeedback protocols for alcohol use disorder may focus on enhancing executive function and emotional regulation, while those for opioid use disorder may target pain processing and reward circuitry. Additionally, neurofeedback interventions can be customized to address co-occurring mental health conditions, such as anxiety or depression, which often accompany substance use disorders. These personalized approaches aim to optimize treatment outcomes by addressing the unique neurophysiological underpinnings of each individual's substance use disorder.